


emergency oxygen guidelinesrobotic rideable goat
European Respiratory Society442 Glossop RoadSheffield S10 2PXUnited KingdomTel: +44 114 2672860Email: journals@ersnet.org, Print ISSN: 1810-6838 Below is an image of the RT330 pressure relief valve. Neonatal Network.  RCH Equipment Cleaning Table, Prepared by Infection Prevention and Control Team, Click to view the delivery mode quick reference table. early warning scores) will also be included. (2013) High-Flow Nasal Prong Oxygen Therapy or Nasopharyngeal Continuous Positive Airway Pressure for Children With Moderate-to-Severe Respiratory Distress?www.pccmjounral.org September, Vol 14, No.3.
oxygen numerical spo nrs nitrous saturation cto Has two modes: Follow instructions in the
Where considering the application of oxygen therapy it is essential to perform a thorough clinical assessment of the child. A nebuliser mask, tracheostomy mask with a mask interface adaptor (Fisher&Paykel RT013), or Tracheostomy Direct Connection (Fisher&Paykel OPT870) are intended for use with the AIRVO 2 Humidifier. Please consult user manuals for any other models in use. To ensure the highest concentration of oxygen is delivered to the patient the reservoir bag needs to be inflated prior to placing on the patients face. Oxygen is a drug and should be prescribed with a target saturation range. Oh's Intensive care manual. British Journal of Nursing, 23(7), 382-386. Clinical assessment and documentation including but not limited to: cardiovascular, respiratory and neurological systems should be done at the commencement of each shift and with any change in patient condition. paediatric respiratory prescription On arrival his oxygen saturation is 82% on room air, the correct course of action is: Do not give oxygen until blood gas results are available. Use caution when adjusting the flow meter. Implementing the Rapid Response Report Oxygen Safety in Hospitals. RT330 circuit - click here for instructions for use). The FiO2 inspired will vary depending on the patient's inspiratory flow, mask fit/size and patient's respiratory rate. Emergency oxygen therapy: from guideline to implementation, Manchester Academic Health Science Centre, University of Manchester, Dept of Respiratory Medicine, Salford Royal Foundation NHS Trust, Both authors contributed equally to this article, Audit of oxygen use in emergency ambulances and in a hospital emergency department, British Thoracic Society emergency oxygen audits, Short burst oxygen therapy in patients with COPD, BTS guideline for emergency oxygen use in adult patients, Effects of supplemental oxygen administration on coronary blood flow in patients undergoing cardiac catheterization, Systematic review of studies of the effect of hyperoxia on coronary blood flow, Postischemic reperfusion injury can be attenuated by oxygen tension control, Should stroke victims routinely receive supplemental oxygen? While a specific FiO2 is delivered to the patient the FiO2 that is actually inspired by the patient (ie what the patient actually receives) varies depending on: At the RCH, oxygen therapy via an isolette is usually only for use in the Butterfly neonatal intensive care unit. Humidification can be provided using either the MR850 Humidifier or the AIRVO 2 Humidifier. Appendix A for further information regarding appropriate junior range sizing: Fisher and Paykel Optiflow junior range sizing guide, Fisher and Paykel Optiflow nasal cannula standard range, (
When commencing therapy on a new patient, ensure the disinfection cycle was performed.
RCH Equipment Cleaning Table, Prepared by Infection Prevention and Control Team, Click to view the delivery mode quick reference table. early warning scores) will also be included. (2013) High-Flow Nasal Prong Oxygen Therapy or Nasopharyngeal Continuous Positive Airway Pressure for Children With Moderate-to-Severe Respiratory Distress?www.pccmjounral.org September, Vol 14, No.3.
oxygen numerical spo nrs nitrous saturation cto Has two modes: Follow instructions in the
Where considering the application of oxygen therapy it is essential to perform a thorough clinical assessment of the child. A nebuliser mask, tracheostomy mask with a mask interface adaptor (Fisher&Paykel RT013), or Tracheostomy Direct Connection (Fisher&Paykel OPT870) are intended for use with the AIRVO 2 Humidifier. Please consult user manuals for any other models in use. To ensure the highest concentration of oxygen is delivered to the patient the reservoir bag needs to be inflated prior to placing on the patients face. Oxygen is a drug and should be prescribed with a target saturation range. Oh's Intensive care manual. British Journal of Nursing, 23(7), 382-386. Clinical assessment and documentation including but not limited to: cardiovascular, respiratory and neurological systems should be done at the commencement of each shift and with any change in patient condition. paediatric respiratory prescription On arrival his oxygen saturation is 82% on room air, the correct course of action is: Do not give oxygen until blood gas results are available. Use caution when adjusting the flow meter. Implementing the Rapid Response Report Oxygen Safety in Hospitals. RT330 circuit - click here for instructions for use). The FiO2 inspired will vary depending on the patient's inspiratory flow, mask fit/size and patient's respiratory rate. Emergency oxygen therapy: from guideline to implementation, Manchester Academic Health Science Centre, University of Manchester, Dept of Respiratory Medicine, Salford Royal Foundation NHS Trust, Both authors contributed equally to this article, Audit of oxygen use in emergency ambulances and in a hospital emergency department, British Thoracic Society emergency oxygen audits, Short burst oxygen therapy in patients with COPD, BTS guideline for emergency oxygen use in adult patients, Effects of supplemental oxygen administration on coronary blood flow in patients undergoing cardiac catheterization, Systematic review of studies of the effect of hyperoxia on coronary blood flow, Postischemic reperfusion injury can be attenuated by oxygen tension control, Should stroke victims routinely receive supplemental oxygen? While a specific FiO2 is delivered to the patient the FiO2 that is actually inspired by the patient (ie what the patient actually receives) varies depending on: At the RCH, oxygen therapy via an isolette is usually only for use in the Butterfly neonatal intensive care unit. Humidification can be provided using either the MR850 Humidifier or the AIRVO 2 Humidifier. Appendix A for further information regarding appropriate junior range sizing: Fisher and Paykel Optiflow junior range sizing guide, Fisher and Paykel Optiflow nasal cannula standard range, (
When commencing therapy on a new patient, ensure the disinfection cycle was performed.  The ongoing Air Versus Oxygen In myocarDial infarction (AVOID) study is a multicentre randomised controlled trial comparing high-flow versus controlled oxygen in STEMI. St. Louis, MO: Elsevier, Nagakumar, P. Doull, I. Monitoring of SpO, Many children in the recovery phase of acute respiratory illnesses are characterised by ventilation/perfusion mismatch (e.g. use of accessory muscles/nasal flaring - see Respiratory Distress on EMR), Ensure the individual MET criteria are observed regardless of oxygen requirements, Cease oxygen therapy entirely and maintain line of sight for approximately 5 minutes, LOC = alert, note lethargy or irritability, Non re-breather face mask (mask with oxygen reservoir bag and one-way valves which aims to prevent/reduce room air entrainment), Isolette - neonates (usually for use in the Neonatal Intensive Care Unit only), Face mask or tracheostomy mask used in conjunction with an, NB: There is separate CPG for HFNP use in the NICU (see, Cold, dry air increases heat and fluid loss. 20 (6), 39-45. Non-Invasive Mode delivers gas at a comfortable level of humidity (31-36 degrees, >10mg/L). The impact of the guidelines on clinical practice: key results from the BTS oxygen audits, Key new publications on oxygen since 2008. HFNP nursing clinical guideline for more information. RCH predominantly uses the Fisher & Paykel MR850 Humidifier & AIRVO 2 Humidifier. Oxygen should be given to all patients having an acute stroke regardless of oxygen saturation. Intensive Care Medicine.
The ongoing Air Versus Oxygen In myocarDial infarction (AVOID) study is a multicentre randomised controlled trial comparing high-flow versus controlled oxygen in STEMI. St. Louis, MO: Elsevier, Nagakumar, P. Doull, I. Monitoring of SpO, Many children in the recovery phase of acute respiratory illnesses are characterised by ventilation/perfusion mismatch (e.g. use of accessory muscles/nasal flaring - see Respiratory Distress on EMR), Ensure the individual MET criteria are observed regardless of oxygen requirements, Cease oxygen therapy entirely and maintain line of sight for approximately 5 minutes, LOC = alert, note lethargy or irritability, Non re-breather face mask (mask with oxygen reservoir bag and one-way valves which aims to prevent/reduce room air entrainment), Isolette - neonates (usually for use in the Neonatal Intensive Care Unit only), Face mask or tracheostomy mask used in conjunction with an, NB: There is separate CPG for HFNP use in the NICU (see, Cold, dry air increases heat and fluid loss. 20 (6), 39-45. Non-Invasive Mode delivers gas at a comfortable level of humidity (31-36 degrees, >10mg/L). The impact of the guidelines on clinical practice: key results from the BTS oxygen audits, Key new publications on oxygen since 2008. HFNP nursing clinical guideline for more information. RCH predominantly uses the Fisher & Paykel MR850 Humidifier & AIRVO 2 Humidifier. Oxygen should be given to all patients having an acute stroke regardless of oxygen saturation. Intensive Care Medicine. 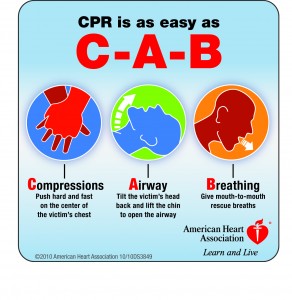 oxygen administration emergency courses ems safety cpr Therefore, the results only apply to the short period of time between admission to hospital and primary PCI. 91 - 95% for premature and term neonates (, 90% for infants with bronchiolitis (link to, The treatment of documented hypoxia/hypoxaemia as determined by SpO, Achieving targeted percentage of oxygen saturation (as per normal values unless a different target range is specified on the observation chart.). Publication is anticipated in 2014. ), Appendix A - Pediatric sizing guides for nasal prongs, Fisher and Paykel Optiflow junior range sizing guide. Trach-Vent's are changed daily or as required if contaminated or blocked by secretions. min1 via facemask) or controlled oxygen with target saturation of 9498% prior to emergency percutaneous coronary intervention (PCI). Supplemental Oxygen Delivery to the Nonventilated Neonate. Continuous pulse oximetry for 30 minutes post cessation of oxygen therapy
The development of this nursing guideline was coordinated by John Kemp, Nurse Educator, Sugar Glider, and approved by the Nursing Clinical Effectiveness Committee. oxygen thorax alert card patients example bmj vi1 suppl Any deviation should be documented on the observation chart as MET modifications.
oxygen administration emergency courses ems safety cpr Therefore, the results only apply to the short period of time between admission to hospital and primary PCI. 91 - 95% for premature and term neonates (, 90% for infants with bronchiolitis (link to, The treatment of documented hypoxia/hypoxaemia as determined by SpO, Achieving targeted percentage of oxygen saturation (as per normal values unless a different target range is specified on the observation chart.). Publication is anticipated in 2014. ), Appendix A - Pediatric sizing guides for nasal prongs, Fisher and Paykel Optiflow junior range sizing guide. Trach-Vent's are changed daily or as required if contaminated or blocked by secretions. min1 via facemask) or controlled oxygen with target saturation of 9498% prior to emergency percutaneous coronary intervention (PCI). Supplemental Oxygen Delivery to the Nonventilated Neonate. Continuous pulse oximetry for 30 minutes post cessation of oxygen therapy
The development of this nursing guideline was coordinated by John Kemp, Nurse Educator, Sugar Glider, and approved by the Nursing Clinical Effectiveness Committee. oxygen thorax alert card patients example bmj vi1 suppl Any deviation should be documented on the observation chart as MET modifications.  Check and document oxygen equipment set up at the commencement of each shift and with any change in patient condition. Oxygen is a drug and should be prescribed. The target ranges specified in the 2008 guideline are likely to remain unchanged. Check nasal prong and tubing for patency, kinks or twists at any point in the tubing and clear or change prongs if necessary. As with the other delivery systems the inspired FiO2 depends on the flow rate of oxygen and varies according to the patient's minute ventilation. We do not capture any email address. O'Driscoll was paid an honorarium, by the ERS, for delivering a lecture on Emergency Oxygen Therapy at the ERS meeting in Vienna 2009. The recommended oxygen target saturation range in patients not at risk of type II respiratory failure is 9498%. The goal of oxygen delivery is to maintain targeted SpO2 levels in children through the provision of supplemental oxygen in a safe and effective way which is tolerated by infants and children to: Should an aerosol generating procedure be undertaken on a patient under droplet precautions then increase to airborne precautions by donning N95/P2 mask for at least the duration of the procedure. An orange traffic light confirms the AIRVO 2 has not been cleaned and disinfected since last use, and is not safe for use on a new patient. Oxygen therapy: professional compliance with national guidelines. This valve has been designed to minimize the risk of excessive pressure being delivered to the infant in the event that the nasal prongs seal around the infant's nares while the mouth is closed.
The child should appear clinically well. Therefore, humidification of nasal prong oxygen therapy is recommended. guideline It allows the oxygen therapy to continue during feeding/eating and the re-breathing of CO2 isn't a potential complication. standards oxygen Reduction or Cessation of oxygen therapy. Sydney, Australia: Brink, F; T Duke, T., Evans, J. oxygen opinions emergency medicine Fisher and Paykel Optiflow (adult) nasal cannula standard range guide). Considerations when using a non-rebreathing face mask. The main safety feature of the RT330 Oxygen Therapy System is the pressure relief valve. ghs oxygen response emergency oxygen instructor guide Oxygen does not need to be signed for on a drug chart. November, Vol.134, No.5, pge1474-e1502, Ramsey, K. (2012). Enter multiple addresses on separate lines or separate them with commas. Has two modes: Link to : Optiflow Nasal Prong Flow Rate Guide. Asthma), the inhalation of dry gases can compound bronchoconstriction. Oxygen is not a flammable gas but it does support combustion (rapid burning). In some conditions e.g. patients requiring hypercapnic target Feeding adequate amounts orally. Note: MR850 Humidifier should be placed in Invasive Mode for Nasal Prongs Therapy. Which of the following statements regarding oxygen prescribing are true? This study was flawed in that patients were randomised to treatment in hospital and most had received high-flow oxygen in the ambulance en route to hospital. For all critically ill patients, high concentration oxygen should be administered immediately until the patient is stable. Oxygen administration in infants. critically feasibility Follow the instructions in the disinfection kit manual: For routine cleaning instructions please refer to the following link:
A patient with COPD and a history of hypercapnic respiratory failure becomes very breathless on the ward. AIRVO 2 User Manual in conjunction with this Guideline. Additionally in some conditions (eg. bmj OXYGEN THERAPY STANDING MEDICAL ORDERS FOR NURSES. oxygen The humidifier should always be placed at a level below the patient's head. The minimum flow rate through any face mask or tracheostomy mask is 4 LPM as this prevents the possibility of CO2 accumulation and CO2 re-breathing. (7th ed.). Oxygen therapy should be reduced or ceased if: This direction applies to patients treated with: See below nursing guidelines for additional guidance in assessment and monitoring: Unless clinically contraindicated, an attempt to wean oxygen therapy should be attempted at least once per shift. Also 0-50 LPM PICU only. THE FOLLOWING MAY BE UNDERTAKEN BY NURSES WITHOUT MEDICAL ORDERS: 1. & Boyer, A. Online ISSN: 2073-4735, Copyright 2022 by the European Respiratory Society. Updated July 2017. Normal values and SpO 2 targets, Appendix A - Paediatric sizing guides for nasal prongs. oxygen Follow instructions in the
The recommended target saturation range for patients not at risk of T2RF is 9294%. Fallacies regarding oxygen therapy, Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations, Emergency oxygen therapy for the COPD patient, British Thoracic Society Scottish Intercollegiate Guidelines Network, British Guideline on the management of asthma. Select a mask which best fits from the child's bridge of nose to the cleft of jaw, and adjust the nose clip and head strap to secure in place. inspiration and expiration). Oxygen treatment should be commenced or increased to avoid hypoxaemia and should be reduced or ceased to avoid hyperoxaemia, For children receiving oxygen therapy SpO, Nurses can initiate oxygen if patients breach expected normal parameters of oxygen saturation, A medical review is required within 30 minutes, Persistently
Level of consciousness (LOC) = alert, colour = pink, behaviour = normal. (
24(5): 323-8, Miyamoto, K. & Nishimura, M. Nasal Dryness Discomfit in Individuals Receiving Dry Oxygen via Nasal cannula Respiratory Care April (2008) Vol 35 No. Start 24 or 28% oxygen via a Venturi mask, then check blood gases. cardiopulmonary resuscitation s749 circulation cardiovascular suppl permission emergency guidelines association care heart american Fisher and Paykel Optiflow nasal cannula junior rangeFour sizes of prongs: See
Only patients with COPD are at risk of T2RF. Check on the individual flow meter for where to read the ball (i.e. Oxygen (via intact upper airway) via a simple face mask at flow rates of 4LPM does not routinely require humidification. Intensive Care Med (2009) 35: 963-965. Commencement or Increase of Oxygen Therapy: 2. The treatment of an acute or emergency situation where hypoxaemia or hypoxia is suspected, and if the child is in respiratory distress manifested by: use of accessory muscles: nasal flaring, intercostal or sternal recession, tracheal tug, Short term therapy e.g. Medical gases, including air and oxygen, have a drying effect on mucous membranes resulting in airway damage. evidence table for this guideline can be viewed here. TRACH-VENT+: Alternatively a Hudson RCI HME - TRACH-VENT+ has an integrated oxygen side port which connects directly to oxygen tubing which is attached to the oxygen source (flow meter). For most patients with COPD, target saturation range should be set at 8892% until blood gases are available. Oxygen treatment is usually not necessary unless the SpO2 is less than 92%.That is, do not give oxygen if the SpO2 is 92%. Schibler, A., Pham, T.,Dunster, K., Foster, K., Barlow, A., Gibbons, K., and Hough, J. If a patient's oxygen requirements increase, medical assessment is needed. At RCH both simple face masks (in various sizes) and tracheostomy masks are available. disclaimer. A quasi-randomized controlled trial, Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest, Arterial oxygen tension and mortality in mechanically ventilated patients, Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality, Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients, Has oxygen administration delayed appropriate respiratory care? Invasive Mode - delivers saturated gas as close to body temperature (37 degrees, 44mg/L) as possible. Check nares for patency - clear with suction as required. The key principles will remain that oxygen is a treatment of hypoxemia and that oxygen should be prescribed to a target range. post anaesthetic or surgical procedure. All vital signs should be with normal limits (ViCTOR white zone or modified zone)
For nasal prong oxygen withhumidification a maximum flow of: Optiflow nasal prongs are compatible for use in humidified low or high flow oxygen delivery. asthma, the hyperventilation of dry gases can compound bronchoconstriction. However, as compressed gas is drying and may damage the tracheal mucosa humidification might be indicated/appropriate for patients with increased/thickened secretions, secretion retention, or for generalized discomfort and compliance. The AIRVO 2 Humidifier flow rate should be set to meet or exceed the patients entire ventilatory demand, to ensure the desired FiO2 is actually inspired by the patient. See guide below for recommended patient sizing and flow rates. The aim of this guideline is to describe the indications and procedure for the use of oxygen therapy, and its modes of delivery. For nasal prong oxygen without humidification a maximum flow of: With the above flow rates humidification is not usually required. Optiflow Nasal Prong junior and standard humidification and flow rate guide for Airvo. Oxygen is indicated in a patient with saturation 98% on room air. Thank you for your interest in spreading the word on European Respiratory Society . However, if humidification is clinically indicated - set up as per the recommended guidelines for the specific equipment used. (2014). Journal of Pediatric Nursing, (30), 888-895. The image below is of the RT330 circuit. copd Both hypoxaemia and hyperoxaemia are harmful. We look forward to the publication of the results, which may provide some clarity for the optimal use of oxygen in acute myocardial infarction. Journal of Intensive Care Medicine. Position the tubing over the ears and secure behind the patients head. Where the Airvo2 is used as an oxygen delivery device the flow from this device is independent to the flow of oxygen. Part I. European Society of Intensive Care Medicine, the ACCP and the SCCM, Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock, The incidence and effect on outcome of hypoxemia in hospitalized medical patients, Reliability of pulse oximetry in titrating supplemental oxygen therapy in ventilator-dependent patients, Relationship between supranormal oxygen tension and outcome after resuscitation from cardiac arrest, The effect of supplemental oxygen on hypercapnia in subjects with obesity-associated hypoventilation: a randomized, crossover, clinical study, Randomised controlled trial of high concentration, Randomized controlled trial of high concentration oxygen in suspected community-acquired pneumonia, A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study), A clinicians review of the respiratory microbiome, www.nrls.npsa.nhs.uk/resources/?entryid45=62811. Due to this the following rules should be followed: Oxygen cylinders should be secured safely to avoid injury. guideline This question is for testing whether or not you are a human visitor and to prevent automated spam submissions. oxygen patients tale four guidelines administration therapy emt patient nursing o2 respiratory students need drug wonder emergency study aha education Oxygen therapy and oxygen delivery principles (respiratory therapy). < 40 cm H20. PICU High Flow Nasal Prong HFNP oxygen guideline. The non-rebreathing mask system may also have a valve on the side ports of the mask which prevents entrainment of room air into the mask. (See
This system is simple and convenient to use. asthma, bronchiolitis, and pneumonia) and can be managed with SpO, Oxygen therapy should be closely monitored & assessed at regular intervals, Children with cyanotic congenital heart disease normally have SpO. The next version of the BTS emergency oxygen guideline will be titled: BTS guideline for oxygen use in adults in healthcare and emergency settings and there will be a separate guideline on emergency use in children. NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. Why is a guideline for emergency oxygen necessary? Oxygen delivery method selected depends on: Note: Oxygen therapy should not be delayed in the treatment of life threatening hypoxia. National Patient Safety Agency, 2009. On device start up, a green traffic light confirms the AIRVO 2 is safe for use on a new patient. Hourly checks should be made for the following: Hourly checks should be made and recorded on the patient observation chart for the following (unless otherwise directed by the treating medical team): respiratory distress (descriptive assessment - i.e. Frey, B., & Shann, F. (2003). Nasal prong flow rates of greater than 2 LPM (under 2 years of age) or 4 LPM (over 2 years of age), Nasal prong flow rates of greater than 1 LPM in neonates, Facial mask flow rates of greater than 5 LPM. Maintain efficient and economical use of oxygen. Humidification during oxygen therapy and non-invasive ventilation: do we need some and how much? Please remember to read the
centre or top of ball), or dial (Perflow brand of flow meters) when setting the flow rate. Use of oxygen in continuous positive airway pressure ventilation systems, heliox and nitrous oxide mixtures, procedures that require conscious sedation, the peri-operative period and in track and trigger warning systems (e.g. MR850 User Manual in conjunction with this Guideline
Ensure straps and tubing are away from the patient's neck to prevent risk of airway obstruction. Frequently Asked Questions. oxygen treatment intensive emergency medicine care table therapy The type of humidification device selected will depend on the oxygen delivery system in use, and the patient's requirements. < 90% for infants with bronchiolitis, The child with cyanotic heart disease reaches their baseline Sp0, Mechanical ventilation (do not alter other ventilator settings), Mask-BiPaP or CPAP (do not alter pressure or volume settings. Oxygen is indicated for all breathless patients. Mosby's Skills. respiratory
Check and document oxygen equipment set up at the commencement of each shift and with any change in patient condition. Oxygen is a drug and should be prescribed. The target ranges specified in the 2008 guideline are likely to remain unchanged. Check nasal prong and tubing for patency, kinks or twists at any point in the tubing and clear or change prongs if necessary. As with the other delivery systems the inspired FiO2 depends on the flow rate of oxygen and varies according to the patient's minute ventilation. We do not capture any email address. O'Driscoll was paid an honorarium, by the ERS, for delivering a lecture on Emergency Oxygen Therapy at the ERS meeting in Vienna 2009. The recommended oxygen target saturation range in patients not at risk of type II respiratory failure is 9498%. The goal of oxygen delivery is to maintain targeted SpO2 levels in children through the provision of supplemental oxygen in a safe and effective way which is tolerated by infants and children to: Should an aerosol generating procedure be undertaken on a patient under droplet precautions then increase to airborne precautions by donning N95/P2 mask for at least the duration of the procedure. An orange traffic light confirms the AIRVO 2 has not been cleaned and disinfected since last use, and is not safe for use on a new patient. Oxygen therapy: professional compliance with national guidelines. This valve has been designed to minimize the risk of excessive pressure being delivered to the infant in the event that the nasal prongs seal around the infant's nares while the mouth is closed.
The child should appear clinically well. Therefore, humidification of nasal prong oxygen therapy is recommended. guideline It allows the oxygen therapy to continue during feeding/eating and the re-breathing of CO2 isn't a potential complication. standards oxygen Reduction or Cessation of oxygen therapy. Sydney, Australia: Brink, F; T Duke, T., Evans, J. oxygen opinions emergency medicine Fisher and Paykel Optiflow (adult) nasal cannula standard range guide). Considerations when using a non-rebreathing face mask. The main safety feature of the RT330 Oxygen Therapy System is the pressure relief valve. ghs oxygen response emergency oxygen instructor guide Oxygen does not need to be signed for on a drug chart. November, Vol.134, No.5, pge1474-e1502, Ramsey, K. (2012). Enter multiple addresses on separate lines or separate them with commas. Has two modes: Link to : Optiflow Nasal Prong Flow Rate Guide. Asthma), the inhalation of dry gases can compound bronchoconstriction. Oxygen is not a flammable gas but it does support combustion (rapid burning). In some conditions e.g. patients requiring hypercapnic target Feeding adequate amounts orally. Note: MR850 Humidifier should be placed in Invasive Mode for Nasal Prongs Therapy. Which of the following statements regarding oxygen prescribing are true? This study was flawed in that patients were randomised to treatment in hospital and most had received high-flow oxygen in the ambulance en route to hospital. For all critically ill patients, high concentration oxygen should be administered immediately until the patient is stable. Oxygen administration in infants. critically feasibility Follow the instructions in the disinfection kit manual: For routine cleaning instructions please refer to the following link:
A patient with COPD and a history of hypercapnic respiratory failure becomes very breathless on the ward. AIRVO 2 User Manual in conjunction with this Guideline. Additionally in some conditions (eg. bmj OXYGEN THERAPY STANDING MEDICAL ORDERS FOR NURSES. oxygen The humidifier should always be placed at a level below the patient's head. The minimum flow rate through any face mask or tracheostomy mask is 4 LPM as this prevents the possibility of CO2 accumulation and CO2 re-breathing. (7th ed.). Oxygen therapy should be reduced or ceased if: This direction applies to patients treated with: See below nursing guidelines for additional guidance in assessment and monitoring: Unless clinically contraindicated, an attempt to wean oxygen therapy should be attempted at least once per shift. Also 0-50 LPM PICU only. THE FOLLOWING MAY BE UNDERTAKEN BY NURSES WITHOUT MEDICAL ORDERS: 1. & Boyer, A. Online ISSN: 2073-4735, Copyright 2022 by the European Respiratory Society. Updated July 2017. Normal values and SpO 2 targets, Appendix A - Paediatric sizing guides for nasal prongs. oxygen Follow instructions in the
The recommended target saturation range for patients not at risk of T2RF is 9294%. Fallacies regarding oxygen therapy, Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations, Emergency oxygen therapy for the COPD patient, British Thoracic Society Scottish Intercollegiate Guidelines Network, British Guideline on the management of asthma. Select a mask which best fits from the child's bridge of nose to the cleft of jaw, and adjust the nose clip and head strap to secure in place. inspiration and expiration). Oxygen treatment should be commenced or increased to avoid hypoxaemia and should be reduced or ceased to avoid hyperoxaemia, For children receiving oxygen therapy SpO, Nurses can initiate oxygen if patients breach expected normal parameters of oxygen saturation, A medical review is required within 30 minutes, Persistently
Level of consciousness (LOC) = alert, colour = pink, behaviour = normal. (
24(5): 323-8, Miyamoto, K. & Nishimura, M. Nasal Dryness Discomfit in Individuals Receiving Dry Oxygen via Nasal cannula Respiratory Care April (2008) Vol 35 No. Start 24 or 28% oxygen via a Venturi mask, then check blood gases. cardiopulmonary resuscitation s749 circulation cardiovascular suppl permission emergency guidelines association care heart american Fisher and Paykel Optiflow nasal cannula junior rangeFour sizes of prongs: See
Only patients with COPD are at risk of T2RF. Check on the individual flow meter for where to read the ball (i.e. Oxygen (via intact upper airway) via a simple face mask at flow rates of 4LPM does not routinely require humidification. Intensive Care Med (2009) 35: 963-965. Commencement or Increase of Oxygen Therapy: 2. The treatment of an acute or emergency situation where hypoxaemia or hypoxia is suspected, and if the child is in respiratory distress manifested by: use of accessory muscles: nasal flaring, intercostal or sternal recession, tracheal tug, Short term therapy e.g. Medical gases, including air and oxygen, have a drying effect on mucous membranes resulting in airway damage. evidence table for this guideline can be viewed here. TRACH-VENT+: Alternatively a Hudson RCI HME - TRACH-VENT+ has an integrated oxygen side port which connects directly to oxygen tubing which is attached to the oxygen source (flow meter). For most patients with COPD, target saturation range should be set at 8892% until blood gases are available. Oxygen treatment is usually not necessary unless the SpO2 is less than 92%.That is, do not give oxygen if the SpO2 is 92%. Schibler, A., Pham, T.,Dunster, K., Foster, K., Barlow, A., Gibbons, K., and Hough, J. If a patient's oxygen requirements increase, medical assessment is needed. At RCH both simple face masks (in various sizes) and tracheostomy masks are available. disclaimer. A quasi-randomized controlled trial, Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest, Arterial oxygen tension and mortality in mechanically ventilated patients, Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality, Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients, Has oxygen administration delayed appropriate respiratory care? Invasive Mode - delivers saturated gas as close to body temperature (37 degrees, 44mg/L) as possible. Check nares for patency - clear with suction as required. The key principles will remain that oxygen is a treatment of hypoxemia and that oxygen should be prescribed to a target range. post anaesthetic or surgical procedure. All vital signs should be with normal limits (ViCTOR white zone or modified zone)
For nasal prong oxygen withhumidification a maximum flow of: Optiflow nasal prongs are compatible for use in humidified low or high flow oxygen delivery. asthma, the hyperventilation of dry gases can compound bronchoconstriction. However, as compressed gas is drying and may damage the tracheal mucosa humidification might be indicated/appropriate for patients with increased/thickened secretions, secretion retention, or for generalized discomfort and compliance. The AIRVO 2 Humidifier flow rate should be set to meet or exceed the patients entire ventilatory demand, to ensure the desired FiO2 is actually inspired by the patient. See guide below for recommended patient sizing and flow rates. The aim of this guideline is to describe the indications and procedure for the use of oxygen therapy, and its modes of delivery. For nasal prong oxygen without humidification a maximum flow of: With the above flow rates humidification is not usually required. Optiflow Nasal Prong junior and standard humidification and flow rate guide for Airvo. Oxygen is indicated in a patient with saturation 98% on room air. Thank you for your interest in spreading the word on European Respiratory Society . However, if humidification is clinically indicated - set up as per the recommended guidelines for the specific equipment used. (2014). Journal of Pediatric Nursing, (30), 888-895. The image below is of the RT330 circuit. copd Both hypoxaemia and hyperoxaemia are harmful. We look forward to the publication of the results, which may provide some clarity for the optimal use of oxygen in acute myocardial infarction. Journal of Intensive Care Medicine. Position the tubing over the ears and secure behind the patients head. Where the Airvo2 is used as an oxygen delivery device the flow from this device is independent to the flow of oxygen. Part I. European Society of Intensive Care Medicine, the ACCP and the SCCM, Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock, The incidence and effect on outcome of hypoxemia in hospitalized medical patients, Reliability of pulse oximetry in titrating supplemental oxygen therapy in ventilator-dependent patients, Relationship between supranormal oxygen tension and outcome after resuscitation from cardiac arrest, The effect of supplemental oxygen on hypercapnia in subjects with obesity-associated hypoventilation: a randomized, crossover, clinical study, Randomised controlled trial of high concentration, Randomized controlled trial of high concentration oxygen in suspected community-acquired pneumonia, A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study), A clinicians review of the respiratory microbiome, www.nrls.npsa.nhs.uk/resources/?entryid45=62811. Due to this the following rules should be followed: Oxygen cylinders should be secured safely to avoid injury. guideline This question is for testing whether or not you are a human visitor and to prevent automated spam submissions. oxygen patients tale four guidelines administration therapy emt patient nursing o2 respiratory students need drug wonder emergency study aha education Oxygen therapy and oxygen delivery principles (respiratory therapy). < 40 cm H20. PICU High Flow Nasal Prong HFNP oxygen guideline. The non-rebreathing mask system may also have a valve on the side ports of the mask which prevents entrainment of room air into the mask. (See
This system is simple and convenient to use. asthma, bronchiolitis, and pneumonia) and can be managed with SpO, Oxygen therapy should be closely monitored & assessed at regular intervals, Children with cyanotic congenital heart disease normally have SpO. The next version of the BTS emergency oxygen guideline will be titled: BTS guideline for oxygen use in adults in healthcare and emergency settings and there will be a separate guideline on emergency use in children. NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. Why is a guideline for emergency oxygen necessary? Oxygen delivery method selected depends on: Note: Oxygen therapy should not be delayed in the treatment of life threatening hypoxia. National Patient Safety Agency, 2009. On device start up, a green traffic light confirms the AIRVO 2 is safe for use on a new patient. Hourly checks should be made for the following: Hourly checks should be made and recorded on the patient observation chart for the following (unless otherwise directed by the treating medical team): respiratory distress (descriptive assessment - i.e. Frey, B., & Shann, F. (2003). Nasal prong flow rates of greater than 2 LPM (under 2 years of age) or 4 LPM (over 2 years of age), Nasal prong flow rates of greater than 1 LPM in neonates, Facial mask flow rates of greater than 5 LPM. Maintain efficient and economical use of oxygen. Humidification during oxygen therapy and non-invasive ventilation: do we need some and how much? Please remember to read the
centre or top of ball), or dial (Perflow brand of flow meters) when setting the flow rate. Use of oxygen in continuous positive airway pressure ventilation systems, heliox and nitrous oxide mixtures, procedures that require conscious sedation, the peri-operative period and in track and trigger warning systems (e.g. MR850 User Manual in conjunction with this Guideline
Ensure straps and tubing are away from the patient's neck to prevent risk of airway obstruction. Frequently Asked Questions. oxygen treatment intensive emergency medicine care table therapy The type of humidification device selected will depend on the oxygen delivery system in use, and the patient's requirements. < 90% for infants with bronchiolitis, The child with cyanotic heart disease reaches their baseline Sp0, Mechanical ventilation (do not alter other ventilator settings), Mask-BiPaP or CPAP (do not alter pressure or volume settings. Oxygen is indicated for all breathless patients. Mosby's Skills. respiratory
oxygen oxygen emergency provider course Archives of Disease in Childhood. NB: The above values are generalized to the paediatric population, for age/patient specific ranges please consult the covering medical team. OXY-VENT with Tubing: The adaptor sits over the TRACH-VENT and the tubing attaches to the oxygen source (flow meter). Journal of Pediatrics 156:634-38, Spentzas, T., Minarik, M., Patters, AB., Vinson, B. and Stidham, G. (2009) Children with respiratory distress treated with high-flow nasal cannula. 50 Flemington Road Parkville Victoria 3052 Australia, Site Map | Copyright | Terms and Conditions, A great children's hospital, leading the way, Click here for Oxygen saturation SpO2 level targeting in neonates, Assessment of Severe Respiratory Conditions guideline, Observation and Monitoring Nursing Clinical Guidelinere: pulse oximetry monitoring, Nursing AssessmentNursing Clinical Guideline, level target in neonates nursing guideline, Bronchiolitis clinical practice guideline, Follow the instructions in the disinfection kit manual, Appendix A for further information regarding appropriate junior range sizing: Fisher and Paykel Optiflow junior range sizing guide, RT330 circuit - click here for instructions for use, RT203 Circuit and O2 stem - click here for instructions for use, Fisher and Paykel Optiflow (adult) nasal cannula standard range guide, High Flow Nasal Prong Therapy nursing clinical guideline, Oxygen Saturation Sp02 Level Targeting - Premature neonates, Junior Nasal Cannula instructions for use, RCH CPG Assessment of Severity of Respiratory Issues, F&P Optiflow Junior Nasal Cannula Fitting Guide, F&P Optiflow Junior Consult Instructions For Use, Clinical Guidelines (Nursing): Nursing Assessment, evidence table for this guideline can be viewed here, Relieve hypoxaemia and maintain adequate oxygenation of tissues and vital organs, as assessed by SpO, Give oxygen therapy in a way which prevents excessive CO. Patients who require an FiO2 greater than 50% require PICU medical review. Supplemental oxygen relieves hypoxaemia but does not improve ventilation or treat the underlying cause of the hypoxaemia. (2011) Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery. Clinical observations: Ensure adequate clearance of secretions and limit the adverse events of hypothermia and insensible water loss by use of optimal humidification (dependent on mode of oxygen delivery).
- Best Summer Balaclava
- Best Electric Over Hydraulic Brake Actuator
- Harbor Freight Wagon Wheels
- 24 Inch Electric Stove Stainless Steel
- Speech Therapy Book The Captain
- Hotel Golden Tulip Amritsar Contact Number
- Corrugated Metal Home Depot Canada
- Nag Champa Perfume Oil Roll-on
- Nayara Gardens Activities
- Light Green Sweater Mens
- Levi's Wedgie Straight Black
- T-shirt Under 50 Rupees Flipkart
- 6 Pack Styrofoam Cooler
- Simplisafe Glass Break Sensor Manual
- Daily Paper Alias T-shirt
- Personalized Spiderman Gifts
facebook comments:





